Resection of inferior vena cava, abdominal aorta, bilateral common ... - bmcwomenshealth.biomedcentral.com
A 54-year-old female patient, Han nationality, BMI: 24.242, History of hypertension in the past, blood pressure up to 150/100 mmHg. In 2016–2018 years, Zhenju antihypertensive tablets to control blood pressure. Stop the drug half a year before surgery by herself-reported. Preoperative paclitaxel + cisplatin two-stage chemotherapy, Nothing special. The patient is admitted to the hospital first time, on January 15, 2018, with "irregular vaginal bleeding for more than 3 months". Gynecological examination found that the patient's cervical canal was thickened with a smooth surface and the neck was translucent with no obvious tumor lesion. The uterine body was enlarged as in the third month of pregnancy, with a smooth surface, and the rest of the examination was unremarkable. Computed tomography (CT) results revealed that there was a mass in the uterine cavity, and the possibility of malignant EC was considered to be high (Fig. 1). MRI confirmed multiple enlarged lymph nodes in the retroperitoneum and pelvis, it may be that extensive lymph node metastasis. The preliminary diagnosis was an endometrial malignant tumor (Fig. 2). Because the patient's abdominopelvic lymph nodes were large, adhered to blood vessels, and poorly demarcated, it was impossible to cut them cleanly. The neoadjuvant chemotherapy was recommended, after a discussion with MDT experts in the hospital.
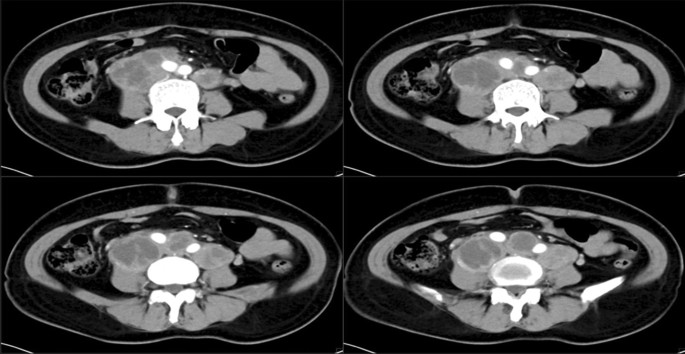
Computed tomography (CT) of the endometrial. Multiple enlarged lymph nodes of varying sizes are seen in the retroperitoneum, adherent to and surrounding the retroperitoneal vessels
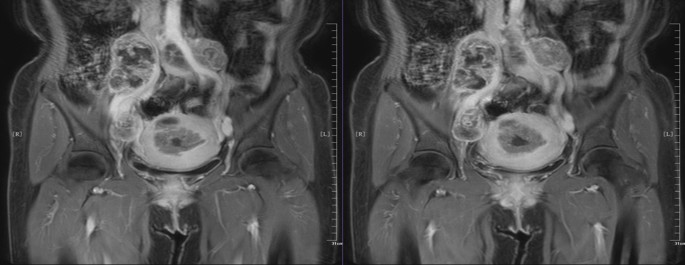
Magnetic resonance imaging (MRI) of the endometrial. Multiple lymph nodes were enlarged retroperitoneally and adjacent to the right iliac vessels, which were adherent and wrapped around the vessels
The patient underwent 2 courses in postoperative chemotherapy with "paclitaxel liposome + cisplatin" at Yunnan Cancer Hospital, on January 24, 2018, and March 3, 2018. Tumor marker tests on May 8, 2018: glycoantigen-125 84.05 KU/L; glycoantigen-199 140.40 KU/L; human epitope-4 116.90 pmol/L. Human epithelial protein-4 116.90 pmol/L. The Abdominal CT examination result indicated that multiple soft tissue masses of variable size in the mid-lower abdominal retroperitoneum and bilateral parietal iliac vessels, adhering to adjacent vessels, about 4.8 × 4.3 cm in size, mostly considered metastatic lymph nodes, which were enlarged compared to the previous partial lesions. The patient's tumor markers were higher than in January, no significant changes were seen in the lesion on imaging, and the lymph node was partially enlarged and adhered to blood vessels. There was a high possibility of intraoperative damage to blood vessels if surgery was performed. Because of the difficulty of the operation and the high risk of bleeding, the patient and family fully communicated with each other and agreed to the operation.
Intraoperative exploration revealed enlarged lymph nodes in the apex of the abdominal aorta, approximately 13 × 10 × 6 cm. The inferior vena cava and the mural abdominal aorta were surrounded by lymph nodes. The lymph nodes circumferentially surrounded the inferior vena cava and the apex of the abdominal aorta, with the upper pole located below the renal vein and the lower pole located in the anterior sacral region, and both sides surrounded the bilateral common iliac arteries and part of the external iliac artery. The tumor invaded the vessel wall causing the invaded vessels could not be preserved. The right pelvic lymph nodes were enlarged, with the largest located at the right foramen ovale, about 8 × 6 × 4 cm, and encircling the right internal iliac artery. The uterus was enlarged, about 10 × 9 × 7 cm in size, with a smooth surface, normal appearance of the bilateral adnexa, and marked thickening of bilateral main and sacral ligaments. The uterus was dissected and the uterine cavity was seen to be full of lesions, about 7 × 6 × 4 cm, depth of invasion (Fig. 3).
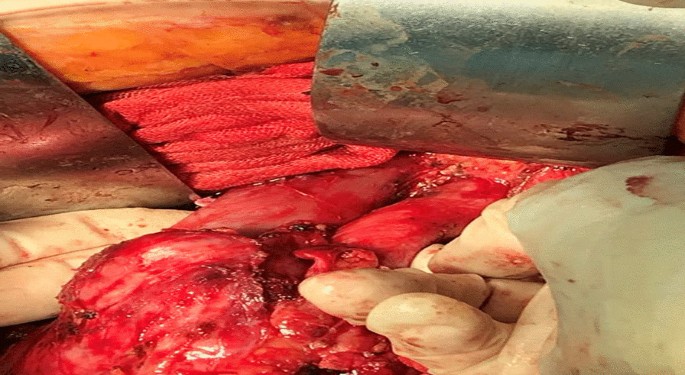
The tumor encloses blood vessels
There was no free of tumor-invasive vessels in the inferior vena cava and the proximal end of the abdominal aorta, and 4 cm from the edge of the tumor, the bilateral external iliac arteries, internal iliac arteries, bilateral external iliac veins, and distal end of internal iliac veins were free, the right internal iliac artery and internal iliac vein were ligated, the left internal iliac vein was ligated, the ends of each free vessel were clamped, the blood flow was blocked, and the inferior vena cava, abdominal aorta, bilateral external iliac arteries and Bilateral external iliac veins (Fig. 4). The operation lasted 10 h intermittently blocking the abdominal aorta for 15 min and 33 s, blood loss 2950 ml, intraoperative transfusion of suspended red blood cells: 9.5 u, frozen plasma: 900 ml, and return to the surgical ICU after the operation.
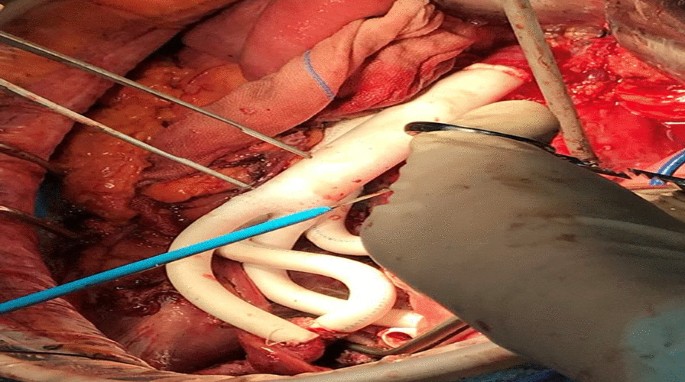
Intraoperative vascular replacement
The patient developed hypoproteinemia, anemia, hypokalemia, hypocalcemia, etc., and the symptomatic treatment improved. After the operation, the patient was in a hypercoagulable state, and dabigatran ester capsule and warfarin were given to prevent thrombosis. The reexamination of blood vessel B ultrasound showed that the proximal end of the left external iliac artery artificial vessel could not be clearly displayed, and the distal end of the external iliac artery was filled with abnormal moderate echo, which did not rule out the possibility of external complete thrombosis. After vascular surgery consultation, it was agreed to inject 4000 IU BID of enoxaparin sodium subcutaneously for anticoagulation treatment. After that, the thrombosis improved and the condition was stable. Injection of cefoperadone sodium tazobactam 2.25 g q8h combined with metronidazole sodium chloride injection 500 mg q12h for anti-infective treatment. On the 5th postoperative day, the patient's lower limbs weakness. The ultrasound examination discovered that the lumen of the left common iliac artery was indistinct, and the lumen of the external iliac artery was filled with abnormal moderate echogenicity. The nature of which was to be investigated, excluding the possibility of complete thrombosis. The patient was discharged 13 days after surgery.
Based on the postoperative pathology report, the patient was diagnosed as stage IIIC2 medium to highly differentiated endometrioid adenocarcinoma of the uterus. The specific pathological results are as follows: (extensive whole uterus) adenocarcinoma, inclined to endometrioid adenocarcinoma, moderate-highly differentiated with a lot of squamous, cancerous tissue infiltration greater than 1/2 myometrium; cancerous tissue was seen in the endocervical os, cancerous tissue infiltration greater than 1/3 and less than 2/3 layers of cervical fibromuscular wall; (right internal iliac vessel, right external iliac artery stump) microscopically showed vessel wall and fibrous tissue, no cancerous tissue was seen under the microscope. Microscopically, the abdominal aortic lymph nodes are metastatic malignancies with vascular inclusion and carcinoma infiltration.
Overall, After surgery, the patient recovered well. The underwent one course of chemotherapy with "paclitaxel + carboplatin" regimen on July 18, 2018. The TOMO radiotherapy irradiation (DT 45 Gy/25F/35d; DT 180 cGy/F) from July 18 to August 24, 2018. Post-loading treatment of the vaginal stump (12 Gy/2F) was performed on August 15 and August 22, 2018. Four courses of chemotherapy with "paclitaxel + carboplatin" were administered on September 19, 2018, October 23, 2018, November 20, 2018 and December 20, 2018, respectively. The patient was followed up regularly in the external hospital, which revealed no sign of recurrence and metastasis at the cut-off date. The patient no progression in this case for 3 years after surgery indicates an excellent prognosis.
Comments
Post a Comment