The Impact of Left Ventricle Ejection Fraction Reduction and ... - Cureus
Introduction: Coronary artery disease (CAD) is a leading cause of death in developed countries. Non-invasive functional imaging modalities are currently recommended as initial diagnostic tests in patients with an intermediate-high pretest probability of CAD. Single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) creates images of regional myocardial tracer uptake, reflecting relative myocardial blood flow. However, there are other non-perfusion predictors of CAD, such as transient ischemic dilatation (TID) and reduced post-stress left ventricle ejection fraction (LVEF). Available data regarding these parameters is controversial. The aim of our study was to evaluate the incidence of significant CAD in patients with non-perfusion high-risk markers of ischemia despite a normal SPECT-MPI.
Methods: Single-center, observational, retrospective, and longitudinal study. Inclusion criteria were age ≥18 years, normal SPECT-MPI, and availability of gated study for LVEF and volume analysis. Exclusion criteria were any known cardiomyopathy or congenital heart disease and known CAD. Non-perfusion high-risk markers: LVEF reduction ≥5% on post-stress images; TID (defined as a stress/rest left ventricle volume ratio ≥ 1.15), including end-systolic, end-diastolic, and mean volumes. The primary endpoint was the identification of significant CAD (stenosis >70% on an epicardial coronary artery or >50% on the left main artery) on invasive coronary angiography.
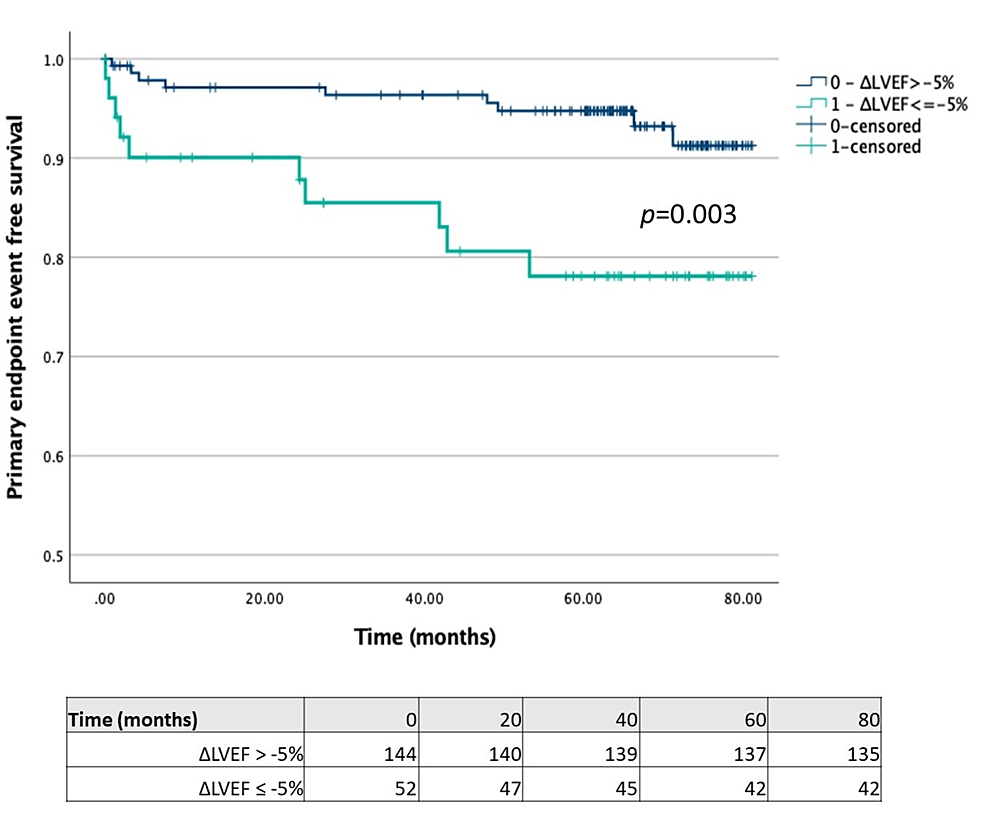
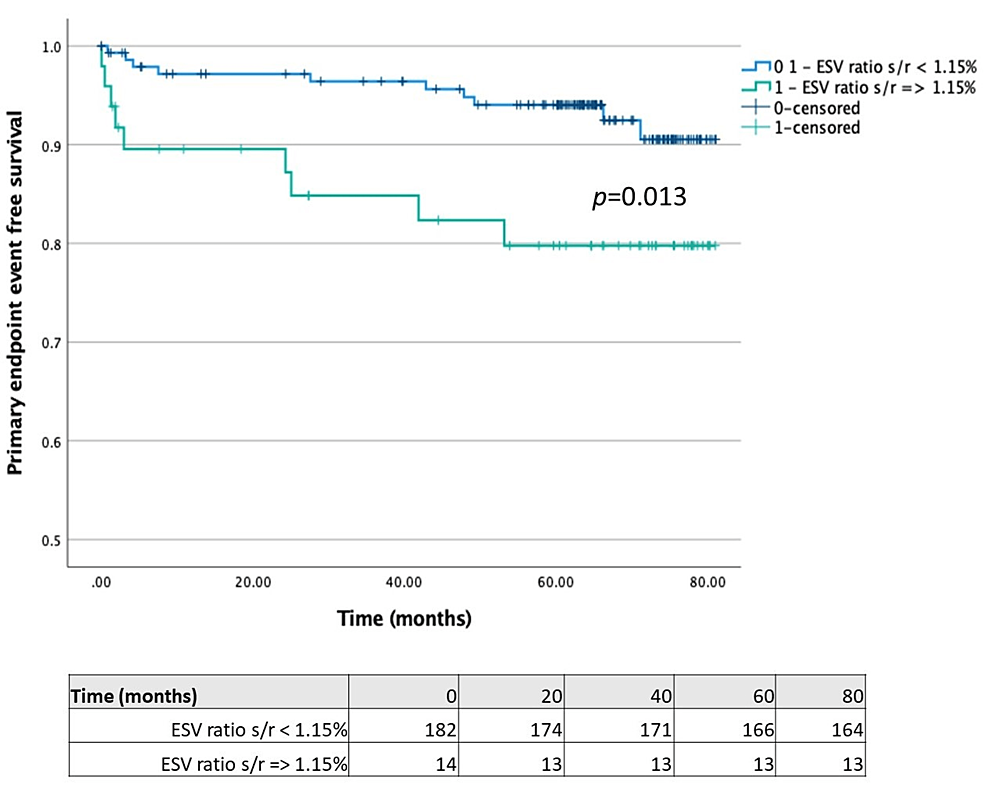
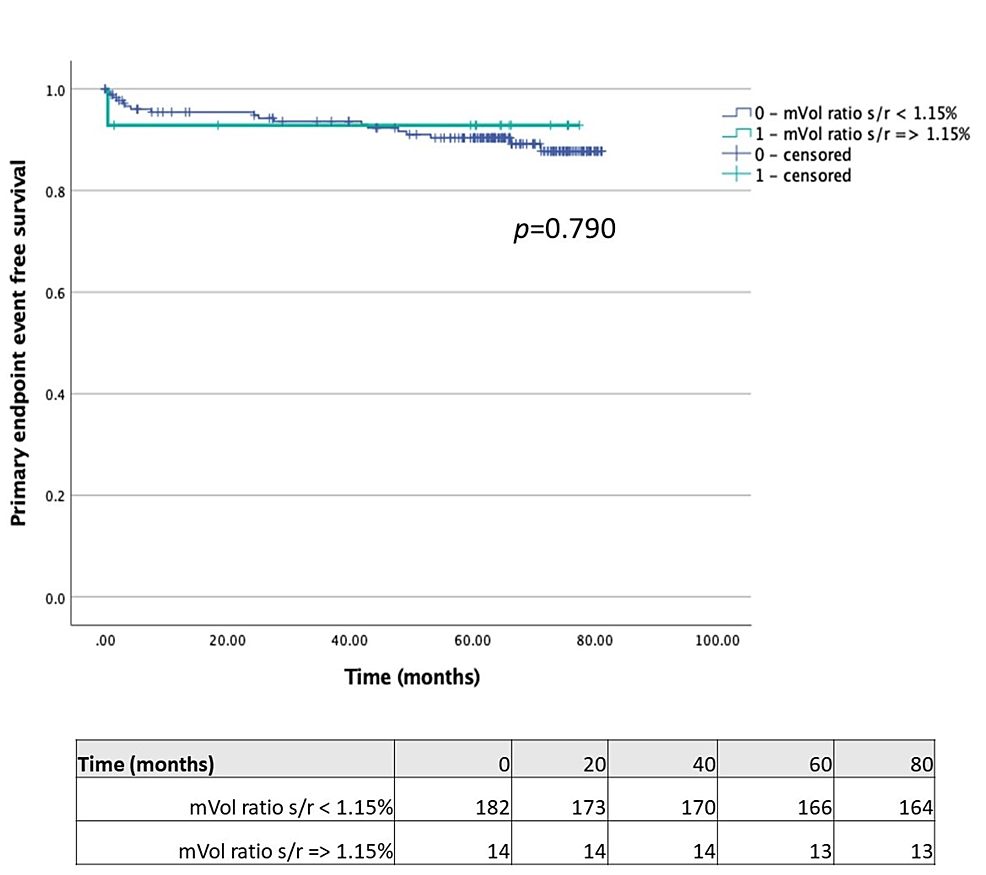
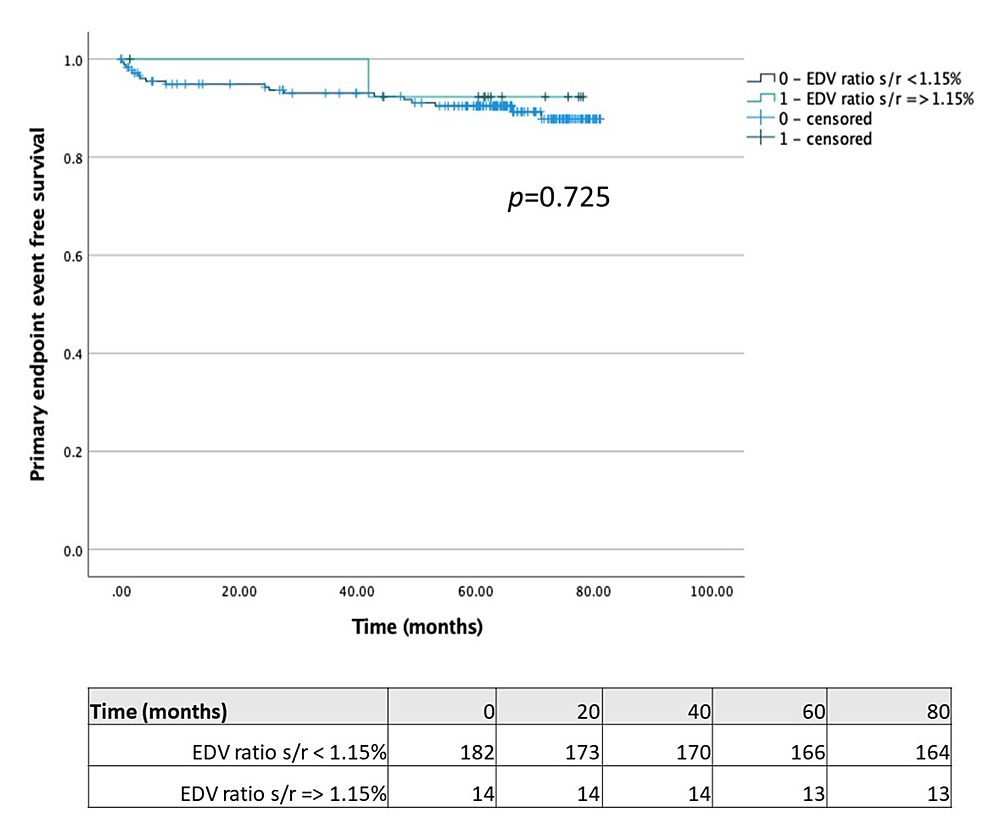
Results: A total of 197 patients met the inclusion criteria. Mean age was 64 ± 12.6 years and 59.4% (n = 117) of patients were male. Overall, 26% of patients had LVEF reduction ≥5% on stress study; 24.9% had a stress/rest end-systolic volume ratio ≥ 1.15; 7.1% had a stress/rest mean volume ratio ≥ 1.15; 7.1% had a stress/rest end-diastolic volume ratio ≥ 1.15. Time-to-primary endpoint was significantly lower in patients with LVEF reduction ≥5% on stress study (67.99 (95% CI 60.49-75.49) vs. 77.56 months (95% CI 75.14-79.99); p = 0.003) and in patients with stress/rest end-systolic volume ratio ≥ 1.15 (68.39 (95% CI 60.69-76.10) vs. 77.31 months (95% ICCI 74.68-79.76); p = 0.013).
Conclusion: In patients with normal perfusion on SPECT-MPI, the incidence of significant CAD was significantly higher in those with LVEF reduction ≥ 5% on stress study and in those with a stress/rest end-systolic volume ratio ≥ 1.15, during a follow-up period of five years.
Introduction
Coronary artery disease (CAD) is a leading cause of death in developed countries, being also a source of significant healthcare-associated costs. Non-invasive functional imaging modalities, such as stress echocardiography, stress cardiac magnetic resonance, single-photon emission computed tomography (SPECT), or positron emission tomography are currently recommended as initial diagnostic tests in patients with an intermediate-high pretest probability of CAD [1].
SPECT myocardial perfusion imaging (SPECT-MPI) creates images of regional myocardial tracer uptake, reflecting relative myocardial blood flow (at rest and during stress), and also providing information regarding the location, extent, and reversibility of perfusion defects [2]. This technique is an important gatekeeper for invasive coronary angiography (ICA) and may provide important information regarding the need for revascularization [3].
Perfusion is the most extensively reported outcome of SPECT. However, there are other non-perfusion predictors of CAD, such as transient ischemic dilatation (TID) and reduced post-stress left ventricle ejection fraction (LVEF). TID is defined as the apparent presence of left ventricular dilation on post-stress relative to rest images; it has been associated with worse cardiovascular outcomes in patients with abnormal SPECT-MPI but has also been linked to balanced ischemia in patients with otherwise normal SPECT-MPI [4-6]. However, data regarding TID in patients with normal SPECT-MPI is controversial. Similarly, although a reduced LVEF in post-stress images has been associated with severe CAD, the literature is also controversial.
The aim of our study was to evaluate the incidence of significant CAD in patients with non-perfusion high-risk markers of ischemia despite a normal SPECT-MPI.
Materials & Methods
Study design and patients
This was a single-center, observational, retrospective, and longitudinal study. Patients were included according to the following criteria: age ≥18 years, normal SPECT-MPI, and availability of gated study for LVEF and volume analysis. Defined exclusion criteria were any known cardiomyopathy or congenital heart disease and known CAD. Outcome data were retrospectively collected in a follow-up period of five years.
Cardiovascular risk factors
The considered cardiovascular risk factors definitions were established according to the current guidelines: hypertension was defined by a systolic blood pressure of ≥140 mmHg, diastolic blood pressure of ≥90 mmHg or use of antihypertensive medication; dyslipidemia was defined as total cholesterol ≥200 mg/dL or use of lipid-lowering medication; diabetes mellitus was defined as hemoglobin A1c levels of ≥6.5% or use of antidiabetic treatment; smoking status was considered only if the patient was currently a smoker. Chronic kidney disease was stated if the glomerular filtration rate was <60 mL/min (stage 3 or higher).
SPECT imaging protocol and definitions
Anti-ischemic drugs were withdrawn before the procedure (48 h for beta-blockers and calcium channel blockers and 6 h for nitrates). The radiotracer was technetium-99m sestamibi. Under continuous electrocardiographic monitoring, treadmill exercise test or adenosine perfusion were used prior to performing gated stress image acquisition. Rest images were acquired in a second moment (same day or a week later).
The 17-segment model was used as a semi-quantitative measurement of radiotracer uptake (0 = normal, 1 = equivocal, 2 = moderate, 3 = severe reduction of uptake, and 4 = absence of detectable tracer). Summed stress score (SSS) was obtained by adding the values of each segment. Normal SPECT-MPI was defined as SSS < 4.
Three-dimensional left ventricle volumes and ejection fractions were derived from local software algorithms. After consulting the available literature, we considered the following two non-perfusion high-risk markers: LVEF reduction ≥5% on post-stress images; TID (defined as a stress/rest left ventricle volume ratio ≥ 1.15), including end-systolic, end-diastolic, and mean volumes [7-9].
Primary endpoint
Primary endpoint was the identification of significant CAD on ICA (stenosis >70% on an epicardial coronary artery or >50% on the left main artery). We compared the incidence of the primary endpoint in patients with and without any of the defined non-perfusion high-risk markers.
Statistical analysis
Continuous variables were expressed as the mean ± standard deviation. The unpaired student's t-test (for normally distributed variables) or the Wilcoxon rank-sum test (for non-parametrically distributed variables) were used to compare groups. Categorical variables were compared using Pearson Chi-squared tests or Fisher exact test for cell counts <6. Kaplan-Meier estimates and long-rank test were used to determine event-free survival and compare groups, respectively.
All statistical analyses were performed using SPSS (Version 28 IBM Corp, Armonk, NY) for Windows. A p-value <0.05 were considered statistically significant and only two-sided tests were conducted.
Results
Baseline characteristics
A total of 197 patients met the inclusion criteria. Baseline characteristics are described in Table 1. Mean age was 64 ± 12.6 years and 59.4% (n = 117) of patients were male. Considering cardiovascular risk factors, 75.6% (n = 149) of patients had hypertension, 54.3% (n = 107) had dyslipidemia, 26.9% (n = 53) had diabetes mellitus, and 14.2% (n = 28) had smoking habits. Also, 14.2% (n = 28) had chronic kidney disease.
SPECT volumetric features
Regarding resting LV systolic function, 11.7% of patients had a baseline LVEF < 50%. Overall, 26.4% of patients had LVEF reduction ≥5% on stress study; 24.9% had a stress/rest end-systolic volume ratio ≥ 1.15; 7.1% had a stress/rest mean volume ratio ≥ 1.15; 7.1% had a stress/rest end-diastolic volume ratio ≥ 1.15.
Time-to-primary endpoint
Comparing patients with LVEF reduction ≥5% on stress study with those without this feature (Figure 1), we found that the former had a significantly lower time-to-primary endpoint (67.99 (95% CI 60.49-75.49) vs. 77.56 months (95% CI 75.14-79.99); p = 0.003). Regarding TID, we separately compared patients with each of the different volume measures (stress/rest mean volume ratio ≥ 1.15, stress/rest end-systolic volume ratio ≥ 1.15 and stress/rest end-diastolic volume ratio ≥ 1.15) with those without the respective features. Although the time-to-primary endpoint was significantly lower in patients with stress/rest end-systolic volume ratio ≥ 1.15 compared with patients without this feature (68.39 (95% CI 60.69-76.10) vs. 77.31 months (95% ICCI 74.68-79.76); p = 0.013) (Figure 2), the same was not observed in patients with stress/rest mean or end-diastolic volume ratios ≥ 1.15 (Figures 3-4).
Discussion
Normal SPECT-MPI has been associated with low rates of cardiac death and non-fatal myocardial infarction (<1%/year) [10]. A recent study by Kassab et al. stated that, compared with patients with normal SPECT-MPI (SSS = 0), patients with near normal perfusion (SSS 1-3) had a higher rate of obstructive CAD, although no difference was found in the incidence of hard cardiac events [11]. The purpose of our study was to evaluate the incidence of significant CAD in patients with non-perfusion high-risk markers of ischemia, namely LVEF reduction on stress study and TID, despite a normal SPECT-MPI.
In our study, LVEF reduction ≥5% was associated with a lower time until the identification of significant CAD on ICA. In individuals devoid of CAD, the normal response to exercise of vasodilator stress should be maintenance or increase in LVEF [12]. Myocardial stunning or severe subendocardial ischemia have been suggested as possible mechanisms behind the post-stress reduction in LVEF [13]. Conflicting results are published regarding the significance of this parameter. For a long time, numerous studies have correlated LVEF reduction with significant CAD on ICA, both in exercise and vasodilator protocols, although most of the featured patients had also abnormal SPECT-MPI [14-17]. In contrast, a study by Gomez et al. concluded that LVEF reduction following regadenoson stress did not predict severe/significant CAD, regardless of MPI findings [7].
Even though the pathophysiology of TID is still in debate, several papers have addressed this topic. In our study, we evaluated stress/rest ratios in end-systolic, end-diastolic, and mean volumes; only TID defined by end-systolic volumes was significantly associated with a lower time-to-primary endpoint. Once again, conflicting results have been published. On one hand, a work by Abidov et al. reported an independent and incremental risk of cardiac events in patients with higher levels of CAD [6]. On the other, Valdiviezo et al. [18] concluded that TID in a normal SPECT-MPI was not associated with severe CAD on ICA; these results were supported by Halligan et al. [4] in a study using correlation with coronary computed tomography angiography.
Our study has several limitations. First, it is a retrospective single-center study, and our population may not represent other realities. Second, the cut-offs used to create the groups were those reported by the available literature. Third, the compared groups were not matched, and the number of individuals in each group is asymmetrical, which may be a source of bias. Also, our endpoint was the identification of significant coronary stenosis on ICA during a follow-up period of five years; during follow-up, the patients that performed ICA likely experienced ischemic symptoms or had an unexplained decrease in LVEF; asymptomatic patients did not perform ICA so that we cannot exclude the presence of asymptomatic but significant coronary lesions. Although we found our results interesting, larger and prospective studies are still needed to further clarify the role of non-perfusion high-risk markers in patients with otherwise normal SPECT-MPI.
Conclusions
In patients with normal perfusion on SPECT-MPI, the incidence of significant CAD was significantly higher in those with LVEF reduction ≥ 5% on stress study and in those with a stress/rest end-systolic volume ratio ≥ 1.15, during a follow-up period of five years.
These markers may be of clinical relevance in the follow-up of patients with suspected CAD.
Comments
Post a Comment