Genome-wide association study of thoracic aortic aneurysm and ... - Nature.com
Abstract
The current understanding of the genetic determinants of thoracic aortic aneurysms and dissections (TAAD) has largely been informed through studies of rare, Mendelian forms of disease. Here, we conducted a genome-wide association study (GWAS) of TAAD, testing ~25 million DNA sequence variants in 8,626 participants with and 453,043 participants without TAAD in the Million Veteran Program, with replication in an independent sample of 4,459 individuals with and 512,463 without TAAD from six cohorts. We identified 21 TAAD risk loci, 17 of which have not been previously reported. We leverage multiple downstream analytic methods to identify causal TAAD risk genes and cell types and provide human genetic evidence that TAAD is a non-atherosclerotic aortic disorder distinct from other forms of vascular disease. Our results demonstrate that the genetic architecture of TAAD mirrors that of other complex traits and that it is not solely inherited through protein-altering variants of large effect size.
Main
TAAD encompass a spectrum of aortic pathology affecting the aortic root, the ascending aorta, the aortic arch and the descending thoracic aorta. Thoracic aortic aneurysms, a dilation of the proximal aorta, are known to progressively enlarge over time, ultimately leading to rupture and death if not surgically repaired. In addition, dissections of the ascending (Stanford type A) or descending (Stanford type B) thoracic aorta are life-threatening conditions requiring emergency treatment, often including surgical repair, and are associated with high short-term and long-term mortality risk1,2. Despite the lethality of these conditions, the genetic determinants of TAAD remain largely unknown, with published GWAS having revealed only four loci reaching genome-wide significance3,4,5. As a result, most of what is understood about the genetics of TAAD has been derived from studies examining rare, pathogenic variants resulting in heritable aortopathy (so called, hereditary TAAD or 'HTAAD')6.
The Million Veteran Program (MVP) is a genomic and precision medicine cohort established in 2011 by the Department of VA Healthcare System to study how genes affect health and disease. We recently demonstrated that a VA Healthcare System-based biobank can aid in the genetic discovery of aortic disease7 and allows for the elucidation of causal biology and mechanisms. Leveraging the MVP resource, we sought to (1) perform a genetic discovery analysis for TAAD across multiple ancestries, (2) explore the spectrum of phenotypes associated with TAAD risk variants through a phenome-wide association study (PheWAS), (3) examine the genetic relationship between TAAD and its epidemiologic risk factors, (4) map causal variants and genes for disease, (5) identify causal tissues and cell types and (6) construct and test a polygenic risk score (PRS) for TAAD (Fig. 1).
In the current study, we first performed a TAAD discovery GWAS in the MVP, with replication from six external datasets. Secondary analyses included a PheWAS of lead TAAD risk variants, MR analyses with known epidemiologic risk factors for disease, a series of analyses to identify causal genes, variants and cell types for TAAD leveraging colocalization techniques and scRNA-seq or snRNA-seq data, and the generation and testing of a TAAD PRS. This figure was created with the assistance of BioRender. Abbreviations: LDL-C, LDL cholesterol; HDL-C, HDL cholesterol; TG, triglycerides; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Results
Common variants associated with TAAD
We designed a two-phased GWAS. The initial MVP discovery analysis was composed of 8,626 individuals (7,050 European, 1,266 African and 310 Hispanic ancestry participants) with TAAD and 453,043 disease-free individuals from the same ancestral groups (Supplementary Fig. 1); their baseline characteristics are presented in Supplementary Table 1. Participants with TAAD were more likely to be older, male, prescribed statin therapy and former smokers.
Through genotype imputation, we obtained 25.4 million, 40.3 million and 34.9 million DNA sequence variants for analysis in participants of European, African and Hispanic ancestry, respectively (Supplementary Table 1). Following multi-ancestry meta-analysis in the discovery phase, a total of 1,465 variants at 25 loci met a genome-wide significance threshold (P < 5 × 10−8; Supplementary Figs. 2 and 3). We replicated the known FBN1 (ref. 3), ULK4 (ref. 4) and LRP1 (ref. 4) loci at genome-wide significance and the recently identified TCF7L2 (ref. 5) locus with P < 5 × 10−5 (Supplementary Table 2). Notably, in the MVP, we found no evidence of association for three variants previously reported in an analysis of 435 thoracic aortic aneurysm cases that lacked independent replication8, suggesting that these rare variant associations may be false positive findings (Supplementary Table 3).
Of the 1,465 variants reaching genome-wide significance in the MVP, 1,461 were also available for independent testing in external datasets (4,459 individuals with TAAD, 512,463 individuals without TAAD across six cohorts of predominantly European ancestry) and were taken forward for replication. Following replication, 21 loci continued to exceed genome-wide significance (P < 5 × 10−8), with the four known and 17 new loci demonstrating a directionally consistent replication P value < 0.05 (Tables 1 and 2 and Supplementary Tables 4 and 5). The FBN1 variant rs1818275 was the most significant association (17.4% frequency for the C allele; odds ratio (OR) = 1.35; 95% confidence interval (CI), 1.41–1.30; P = 2.5 × 10−47). All five signals that did not replicate failed to meet the pre-specified threshold (P < 0.05) for independent replication (Supplementary Table 6).
Of the 21 TAAD risk loci, 16 were directionally consistent across European, African and Hispanic ancestries in the MVP; 13 demonstrated at least nominal significance (two-sided P < 0.05) in individuals of African ancestry, and six did likewise in participants of Hispanic ancestry (Supplementary Table 7). A conditional analysis with GCTA-COJO9 and an ancestry-matched linkage disequilibrium (LD) reference panel identified a total of five additional independent variants across the 21 replicated TAAD GWAS loci (Supplementary Table 8).
Anatomic distribution of TAAD risk variants
We next explored whether the identified TAAD risk variants were associated with a specific anatomic distribution of aortic disease. We examined the 21 TAAD risk variants for association with ascending or descending thoracic aortic diameters in recently published UK Biobank summary statistics from Pirruccello et al. (n = 39,688 individuals)10. We found that all 21 lead variants demonstrated an association with ascending aortic diameter with Bonferroni P < 0.0012 (Fig. 2a,b and Supplementary Table 9). By contrast, only 13 of the 21 variants surpassed this threshold in their association with descending thoracic aortic diameter. We then examined the genome-wide significant aortic diameter loci from Pirruccello et al.10 within our TAAD summary statistics. Of the ascending and descending aortic diameter loci available for testing in our dataset, 49 of 81 and 12 of 46 demonstrated evidence of association with TAAD after Bonferroni correction (P < 0.0004), respectively (Supplementary Table 10).
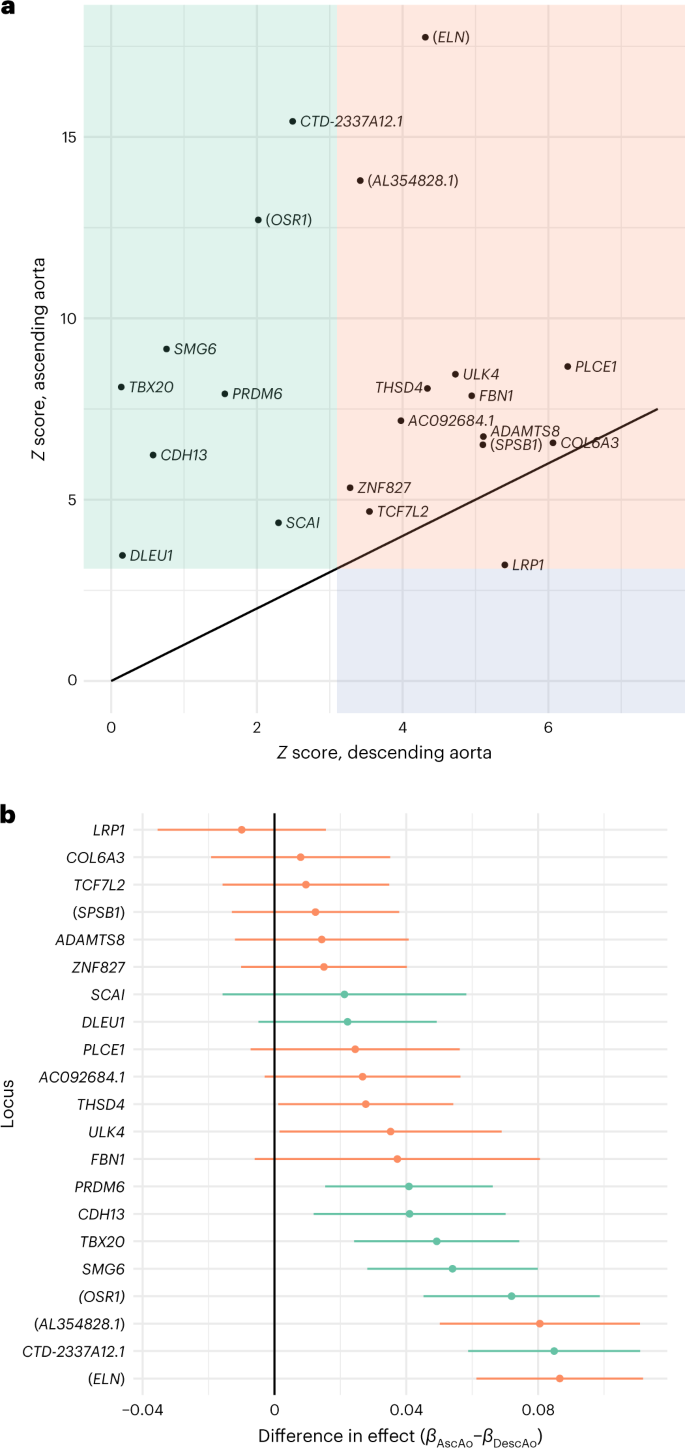
a, Descending aortic diameter Z scores (x axis) and ascending aortic diameter Z scores (y axis) for the 21 TAAD lead risk variants in our study queried in previously published summary statistics from the UK Biobank10 (n = 39,688 individuals). b, Difference in effect estimates (βascending – βdescending) and associated 95% CIs (error bars) for the 21 TAAD lead risk variants in our study queried in previously published summary statistics from the UK Biobank10 (n = 39,688 individuals). AscAo, ascending aorta; DescAo, descending aorta. Variants were declared to be significantly associated with the respective diameter if the linear mixed-model two-sided P value of association was <0.0012. Variants significantly associated with the diameter of the ascending aorta (green), the descending aorta (blue) or both ascending and descending aortic diameters (orange) are displayed.
Phenotypic consequences of TAAD risk variants
Understanding the full spectrum of phenotypic consequences of a given DNA sequence variant can help identify the mechanism by which a variant or gene leads to disease. Termed PheWAS, this approach examines the association of a risk variant across a range of phenotypes11,12. Using data from the Integrative Epidemiology Unit (IEU) OpenGWAS project13,14, we performed a PheWAS of the 21 TAAD lead risk variants across a range of over 2,000 conditions, diseases and metabolites. In total, we identified 167 statistically significant (P < 5.0 × 10−8) PheWAS associations across the 21 genetic variants. In particular, several of the TAAD risk variants were associated with a range of anthropometric traits such as height and conditions including asthma and migraine with genome-wide significance (Supplementary Table 11). Notably, for seven of the 21 variants, the TAAD risk allele was associated with increased diastolic blood pressure (DBP), and three variants demonstrated an association with increased height. By contrast, for all nine variants that demonstrated an association with systolic blood pressure (SBP), the TAAD risk allele was associated with decreased SBP.
Because increased blood pressure and increased height have been reported to be risk factors for TAAD15, we performed a sensitivity analysis retesting the association of the seven DBP-associated variants and three height-associated variants with TAAD, accounting for DBP and height in the association model, respectively (Supplementary Methods). For DBP, while a minor decrease in the TAAD-association P value was observed, in each case, the P value remained significant at the genome-wide level, suggesting that blood pressure was not the primary mediator for the observed genetic association (Supplementary Table 12). For height, all three variants demonstrated an attenuation in association point estimate and P value, although this signal did not completely disappear, suggesting that some, but not all, of the association may be mediated through an increase in standing height (Supplementary Table 13).
Causal epidemiologic risk factors for TAAD
In observational studies, smoking, hyperlipidemia, hypertension and standing height have been suggested as independent risk factors for TAAD15,16. We performed Mendelian randomization (MR) analyses using genetic instruments for a lifetime smoking index17, lipids (triglycerides, high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol)18, blood pressure (SBP, DBP, pulse pressure (PP) and mean arterial pressure (MAP) (https://pan.ukbb.broadinstitute.org)) and height19 (Supplementary Table 14). Consistent with the epidemiologic literature, we observed that a 1-s.d. genetic increase in lifetime smoking index, DBP, MAP and height was associated with increased risk of TAAD (OR, 1.42 for smoking ~20 cigarettes a day for 15 years and stopping 17 years ago; 95% CI, 1.14–1.77; P = 0.002; OR, 1.32 per 10-mmHg increase in DBP; 95% CI, 1.22–1.43; P = 3.0 × 10−12; OR, 1.17 per 10-mmHg increase in MAP; 95% CI, 1.10–1.25; P = 6.9 × 10−7; OR, 1.23 per 7.6-cm increase in height; 95% CI, 1.15–1.33; P = 3.0 × 10−8, two-sided Bonferroni P < 0.0055 (Fig. 3 and Supplementary Fig. 4–6)). Conversely, a 1-s.d. genetic increase in PP was associated with a decreased risk of TAAD (OR, 0.65 per 10-mmHg increase in PP; 95% CI, 0.60–0.71; P = 1.9 × 10−20). Our results remained robust to multiple sensitivity analyses, including the weighted median20 as well as MR-PRESSO21 and MR-Egger22 tests for evidence of horizontal pleiotropy, although MR-PRESSO outlier-corrected results demonstrated effect estimates slightly smaller in magnitude (Supplementary Table 15a). We did not detect a significant association between a genetic 10-mmHg increase in SBP and TAAD risk or an association between any lipid fraction and TAAD.
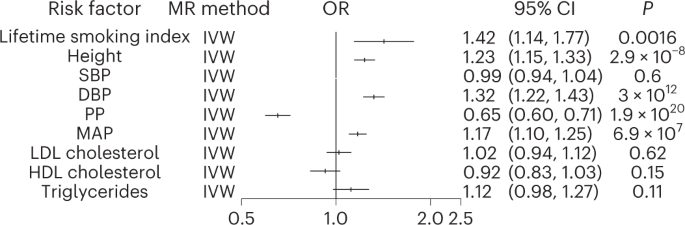
Logistic regression (inverse-variance-weighted; IVW) association results for multiple epidemiologic risk factor exposures with the TAAD outcome in two-sample MR analyses. The lifetime smoking TAAD OR reflects a per-genetic increase in smoking ~20 cigarettes a day for 15 years and stopping 17 years ago. The OR for height reflects a 1-s.d. genetic increase in standing height (~7.6 cm). The SBP, DBP, MAP and PP ORs correspond to the change in TAAD risk per 10-mmHg increase in the blood pressure trait. The lipid ORs reflect the change in TAAD risk per s.d. genetic increase in lipid fraction. Two-sided P values are displayed, and we set a two-sided P < 0.0055 (0.05 ÷ 9 traits) for statistical significance. Error bars represent 95% CIs of the displayed ORs.
Given the substantial overlap in risk variants associated with each blood pressure trait as well as their strong genetic correlation, we next performed an MR Bayesian model-averaging (MR-BMA) analysis, a recently developed analytic tool that applies Bayesian principles to prioritize causal risk factors among correlated exposures with shared genetic predictors (in this case, blood pressure traits)23. MR-BMA generates a marginal inclusion probability that prioritizes causal risk factors for disease rather than determining effect estimates for each of the blood pressure traits on TAAD risk. Genetic instruments were constructed from independent genetic variants associated with any major blood pressure-related trait (SBP, DBP, PP or MAP) at a genome-wide significance level (P < 5 × 10-8, R2 < 0.001). PP and DBP emerged as the most highly prioritized causal blood pressure traits for TAAD risk (PP marginal inclusion probability = 0.82, PNyholt = 2.0 × 10−5; DBP marginal inclusion probability = 0.68, PNyholt = 5.4 × 10−3; Supplementary Table 15b).
Identification of candidate causal TAAD risk genes
We next sought to identify causal TAAD risk genes and variants. Prior human genetic evidence strongly suggests that FBN1 (ref. 24), ELN25 and LRP1 (refs. 26,27) are the causal genes at three of the identified loci, and a recent report provided evidence that TCF7L2 is the likely causal gene acting at the locus5 (Supplementary Table 16). For the remaining loci, we examined the genetic literature and possible causal variants that result in a protein-altering consequence in high LD with the lead variant (R2 > 0.8). In addition, we hypothesized that TAAD risk variants may be acting by inducing expression changes locally in the proximal aortic wall and performed a fine-mapping transcriptome-wide association study (TWAS)28 and colocalization analyses using aortic expression quantitative trait locus (eQTL) data from the Genotype–Tissue Expression Project (GTEx)29. When combining the above strategies, we identified seven additional putative causal genes: THSD4, COL6A3, CDH13, NOC3L, SCAI, PRDM6 and ADAMTS8 (Supplementary Tables 16 and 17). At five of the putative causal genes, we were also able to fine map the locus to five or fewer causal variants (Supplementary Table 18).
Notably, we observed that decreased THSD4 expression was associated with an increased risk of TAAD. The protein product of THSD4, ADAMTSL6, is a known microfibril-associated protein that promotes fibrillin-1 matrix assembly30. In a recent report, rare deleterious THSD4 variants segregated in families with a history of thoracic aortic aneurysms, and Thsd4+/− mice were found to have progressive thoracic aortic dilation31. In sum, these results suggest that common THSD4 variants may cause TAAD through diminished gene expression in the thoracic aorta.
Gene expression analyses reveal TAAD-relevant cell types
We next sought to identify the critical tissues and cell types for TAAD risk variants. At the genome-wide level, we first used stratified LD score regression32 to identify TAAD-relevant tissues and cell types. We combined publicly available expression data from GTEx29 and an aggregation of microarray gene expression datasets comprising 37,427 samples in human, mouse and rat32 (previously referred to as the 'Franke lab dataset') to evaluate for significant enrichment of specific tissues or cell types with genetic TAAD risk-association signals across 205 different tissues and cell types. Not surprisingly, the aorta demonstrated the strongest enrichment (Penrichment = 6.2 × 10−6; Supplementary Table 19). Interestingly, we also observed an enrichment for the uterine myometrium, chondrocytes and osteoblasts (Bonferroni Penrichment < 0.002). Human myometrium is primarily composed of smooth muscle cells, consistent with the well-recognized critical role of vascular smooth muscle cells (VSMCs) in TAAD pathogenesis. Much like fibroblasts, chondrocytes produce and maintain collagen and proteoglycans, and, in cell culture, osteoblasts are nearly indistinguishable from fibroblasts33, providing evidence for a key role of fibroblasts in TAAD development.
We next examined whether a putative causal TAAD risk gene set demonstrated a significant cell type enrichment. We generated a gene set of 21 putative causal TAAD risk genes: the 11 candidate causal genes identified from our GWAS as well as ten additional previously identified definitive or strong HTAAD genes ('category A')6. Of note, FBN1 was present both in our GWAS gene set and in the HTAAD gene set. We then tested whether the 21 putative causal TAAD risk genes were enriched in specific cell types identified from publicly available single-nuclear RNA-sequencing (snRNA-seq) expression data from ascending and descending thoracic aorta10. Using the Fast Gene Set Enrichment software34, we observed that the causal TAAD gene set was significantly enriched in VSMCs (P = 0.0078), and a suggestive enrichment was also observed with fibroblasts (P = 0.02), although this was no longer significant after Bonferroni correction (P < 0.01 = 0.05 ÷ 5 cell types; Supplementary Table 20). These findings are consistent with our results from the stratified LD score regression analysis highlighting VSMCs and fibroblasts as causal TAAD cell types.
Finally, we sought to identify relevant cell types for the individual putative causal TAAD risk genes leveraging single-cell RNA-sequencing (scRNA-seq) data from normal and aneurysmal ascending aortic aneurysm tissue35 and snRNA-seq data from normal ascending and descending thoracic aortas10. For the nine genes that we hypothesized promote TAAD risk through changes in aortic gene expression ('candidate causal genes through changes in expression' in Supplementary Table 17), we first qualitatively assessed for a prioritized cell type (1) the percentage of cells expressing the gene in a given cell type cluster and (2) the magnitude of average gene expression in each cell type (Fig. 4a–c). We then tested the differential expression of each gene among putative cell type clusters between ascending aortic aneurysm and normal aortic tissue samples using Seurat36 (Fig. 4d,e). Integrating this evidence, we prioritized a series of causal cell types for each gene (Fig. 4f). For example, COL6A3 was prioritized to be acting in fibroblasts, consistent with a reported involvement in smooth muscle cell–elastin contact within the aortic wall37. CDH13 (encoding cadherin 13) was prioritized to be acting in fibroblasts, mesenchymal–stromal cells and endothelial cells. Cadherin 13 signaling has been shown to be protective for endothelial cells in the setting of oxidative stress38, and its reported role in angiogenesis39 suggests that it may play a role in aortic remodeling during aneurysmal degeneration across multiple cell types. In total, we prioritized at least one candidate causal cell type for eight of the nine genes thought to be acting through changes in gene expression in the thoracic aorta.
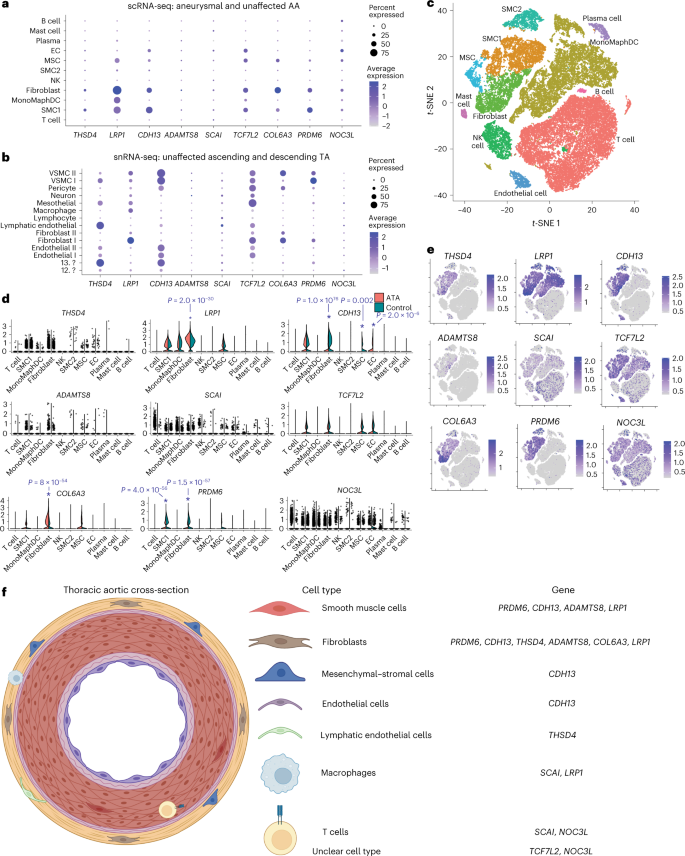
Dot plots for each of the nine candidate causal genes likely affecting TAAD risk based on changes in gene expression in scRNA-seq data from aneurysmal and unaffected ascending aortas35 (a) and snRNA-seq data from unaffected ascending and descending thoracic aortas10 (b). c, t-distributed stochastic neighbor embedding (t-SNE) plot of cell type clusters for scRNA-seq data from aneurysmal and unaffected ascending thoracic aortas. Violin plots (d) and relative expression (e) of each of the nine candidate causal genes likely affecting TAAD risk based on changes in gene expression for each cell type. *Two-sided P value < 0.005 after Bonferroni correction for the maximum number of tests in each cluster (nine) when performing the Wilcoxon rank-sum test for differential expression in aneurysmal ascending thoracic aortic tissue versus unaffected tissue35. f, Prioritized cell type(s) for each of the nine candidate causal genes above depicted along a representative thoracic aortic cross-section. This figure was created with the assistance of BioRender. Abbreviations: AA, ascending aorta; TA, thoracic aorta; ATA, ascending thoracic aneurysm; scRNA-seq, scRNA-seq data; snRNA-seq, snRNA-seq data; SMC, smooth muscle cell; MonoMaphDC, monocyte–macrophage–dendritic cell; NK, natural killer cell; EC, endothelial cell; ?, unclear cell type as referenced10; MSC, mesothelial cell or mesenchymal–stromal cell.
PRS generation for TAAD
Lastly, we sought to examine the contribution of polygenic inheritance on TAAD risk. We generated TAAD PRS including 1,189,073 variants from the MVP discovery GWAS summary statistics (8,626 multi-ancestry TAAD cases, 453,043 controls) and an LD panel from 1000 Genomes40 whole-genome-sequencing data. To increase the number of independent variants included in our score, we used the PRS-CSx software, which uses Bayesian methods to generate posterior genetic variant effect sizes under coupled continuous shrinkage priors41. We first validated the PRS using prevalent data from the Mass General Brigham Biobank (775 cases, 24,518 controls of European ancestry). We observed that the TAAD PRS was strongly associated with prevalent TAAD, with a 1-s.d. increase in PRS associated with a 57% increased risk of disease (ORPRS = 1.57, 95% CI = 1.46–1.69, PPRS = 4.6 × 10−32). Individuals with a PRS in the 95th percentile or higher were 2.67 times more likely to be diagnosed with TAAD (OR = 2.67, 95% CI = 2.11–3.39, PPRS = 6.3 × 10−16; Fig. 5a). After this initial validation step, we then tested this PRS in two additional cohorts.
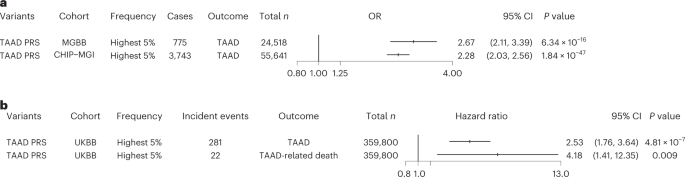
a, Logistic regression ORs and two-sided P values for the association of the top 5% of the TAAD PRS with prevalent TAAD in the Mass General Brigham and CHIP–MGI biobanks. Results were combined in an inverse-variance-weighted fixed-effect meta-analysis. b, Hazard ratios and two-sided P values for the association of the top 5% of the TAAD PRS with incident TAAD and TAAD-related death in the UK Biobank. Error bars represent 95% CIs of the displayed ORs. Abbreviations: MGBB, Mass General Brigham Biobank; UKBB, UK Biobank.
We first assessed the performance of the PRS in individuals of European ancestry in the Cardiovascular Health Improvement Project–Michigan Genomics Initiative (CHIP–MGI) cohort (3,743 cases and 51,898 controls). We again observed an effect estimate greater than 2.0 for the top 5% PRS (OR = 2.28, 95% CI = 2.03–2.56, PPRS = 1.8 × 10−47; Fig. 5a). We next restricted the data to those individuals with targeted or exome sequencing available (1,842 cases and 1,887 controls) and compared the increase in area under the curve (AUC) afforded from the PRS and a set of rare TAAD risk variants that were manually curated as 'pathogenic or likely pathogenic' for HTAAD according to American College of Medical Genetics and Genomics best practices42. While the effect estimate of these pathogenic variants was substantially larger than that observed for the top 5% PRS (ORpathogenic = 11.1; P = 1.4 × 10−10), we noted that, when modeling TAAD risk, the addition of the PRS improved the AUC value by a similar amount as the presence of a pathogenic TAAD risk variant (Supplementary Table 21 and Supplementary Fig. 7). In a sensitivity analysis, we noted similar results when considering rare, deleterious variants as defined by missense variants with a REVEL43 score >0.5 or a LOFTEE44 high-confidence predicted loss-of-function variant within one of the 11 HTAAD genes.
We then sought to examine whether the TAAD PRS was associated with an increase in incident TAAD and incident TAAD-related mortality. Using the UK Biobank, we first tested the PRS with all incident TAAD events and then tested the PRS with incident TAAD events listed as a primary or secondary cause of death in the electronic health record (EHR) using Cox proportional hazard models. We observed that those in the top 5% of the PRS were 2.5-fold more likely to experience an incident TAAD event during a median of 11.2 years of follow up and demonstrated more than fourfold higher risk of TAAD-related mortality (Fig. 5b).
Discussion
In the current study, we identified 17 new TAAD loci and localized the anatomic distribution of these TAAD risk variants. We examined the phenotypic consequences of TAAD lead risk variants with PheWAS, and, through MR, we demonstrate that elevated PP and DBP, taller standing height and smoking are likely causal epidemiologic risk factors for TAAD. Leveraging bulk and scRNA-seq and snRNA-seq data, we identified causal tissues and cell types for TAAD. Lastly, we developed a genome-wide PRS for TAAD that identifies a subset of the population at substantially greater risk for TAAD.
These findings permit several conclusions. First, we provide substantial evidence that the genetic architecture of TAAD mirrors that of other complex traits. Current understanding of the pathophysiology of TAAD has largely been informed through the investigation and identification of rare deleterious variants within what are now termed HTAAD genes. These identified genetic variants, generally missense or nonsense mutations, substantially alter a gene's protein product and subsequently disrupt critical functions in VSMC contraction, extracellular matrix stabilization or transforming growth factor (TGF)-β signaling6. While prior GWAS have identified four TAAD risk loci3,4,5, given the relatively rare incidence of TAAD in the population, it remained unclear whether common or rare variants were the primary driver of TAAD heritability. In the current study, we increase the number of TAAD risk loci by a factor of five and identify putative causal risk genes that likely affect disease through changes in gene expression, akin to other common complex traits. These findings offer new potential targets for therapeutic intervention as well as firmly establish TAAD as a complex trait.
Second, despite its morphologic similarities with infrarenal abdominal aortic aneurysm, our results support the notion that TAAD is a distinct disorder from the rest of the atherosclerotic cardiovascular disease spectrum. Early observational studies of TAAD often studied abdominal and thoracic aortic aneurysms together16, and suggested common risk factors for both diseases included hypertension, smoking and hyperlipidemia. While an association between atherosclerosis and ascending aortic aneurysms has been observed45, whether the two pathologic processes share underlying causal mechanisms remained unknown. Here, through causal inference methods, we provide genetic support for a causal role of smoking and hypertension on TAAD risk. However, unlike for abdominal aortic aneurysm46,47 and other cardiovascular diseases48,49, circulating lipoproteins do not appear to play a substantial role in TAAD development. The loci revealed in our genetic discovery analysis highlight the role of extracellular matrix integrity in TAAD, and the tissue and cell type enrichment analyses underscore the importance of VSMCs in TAAD risk. Prior lineage-mapping studies suggest that the embryologic origin of VSMCs in the thoracic aorta differing from that of the rest of the arterial tree may play a role in susceptibility to atherogenic conditions50. In light of these findings, we hypothesize that therapies focusing on restoring extracellular matrix stability rather than on atherosclerotic risk factor modification will be more likely to provide a substantial impact on TAAD prevention.
Third, our data provide additional evidence for the clinical utility of TAAD PRSs. Although recent literature focusing on PRS application has demonstrated an ability to risk stratify the population at large51, critics have highlighted that this research has focused on diseases in which genetic testing is seldom indicated52, unlikely to substantially alter clinical outcomes53, or that may not be justified within current healthcare cost structures7. However, unlike other diseases, testing for heritable causes of TAAD is already performed, typically through exome sequencing in those with familial or early-onset TAAD syndromes to identify pathogenic variants54. Here, we demonstrate that individuals within the upper tail of the PRS distribution are at substantially greater risk to experience TAAD or TAAD-related mortality. Furthermore, we observed similar gains in the calculated AUC statistic when adding pathogenic or likely pathogenic TAAD risk variants or PRSs (TAAD PRS) to risk-prediction models, suggesting that there is an additional benefit for PRS testing to include common variation beyond current targeted or exome-sequencing panels. In sum, our data suggest that extending current genetic panels to include testing for polygenic TAAD risk may be warranted and deserves further study.
Our study should be interpreted in the context of its limitations. First, our TAAD phenotype is based on EHR diagnosis and procedural code data and may result in misclassification of case status. However, such misclassification should, on average, reduce statistical power for discovery and bias results toward the null. Second, the VA Healthcare System population is overwhelmingly male, and our ability to detect sex-specific genetic associations in discovery was limited. Third, power to detect differential expression associations and identify causal TAAD cell types in scRNA-seq and snRNA-seq data may be limited by sequencing depth, sample size or tissue-processing techniques. Fourth, while we observe a significant MR result for height exposure and TAAD, we cannot rule out the possibility that this association is driven by the pleiotropy of height-associated variants55, rather than a true causal association. Similarly, when examining the scatterplots for each of the significant MR associations, it is possible that the positive results may not necessarily be attributable to a true causal effect but rather that the MR association results may reflect shared biological pathways between the risk factor and TAAD. Finally, a number of the TAAD risk loci demonstrate genome-wide significant associations with increased DBP. Our MR results support a causal role for DBP in TAAD susceptibility; however, our sensitivity analysis suggests that DBP is not the sole driver of TAAD risk at these regions of the genome. Disentangling the effects of hypertension on proximal aortic dilation and dissection, a pathologic process that alters human blood pressure homeostasis, is likely to require model systems to completely elucidate the complex mechanisms at work.
In conclusion, our data provide new mechanistic insights into TAAD risk and demonstrate that its genetic architecture is akin to that of other complex traits. We identify causal risk factors, cell types and genes that may be used to inform clinical care.
Methods
Study populations
We conducted a discovery genetic association analysis using DNA samples and phenotypic data from the MVP (Supplementary Fig. 1). In the MVP, individuals aged 18 to over 100 years have been recruited from 63 VA medical centers across the United States. After quality control, we identified 7,050 participants of European, 1,266 participants of African and 310 participants of Hispanic ancestry with TAAD and 453,043 controls free of clinical evidence of disease. For variants meeting genome-wide significance (P < 5 × 10−8) in the MVP, we sought replication of our findings with data from a meta-analysis of six external datasets comprising 4,459 TAAD cases and 512,463 controls (Supplementary Table 22). Additional details of the MVP and replication genetic data and quality control are available in the Supplementary Information.
TAAD phenotype definitions
From the participants passing quality control in the MVP, individuals were defined as having TAAD based on possessing at least two of the ICD-9 or ICD-10 codes or CPT codes outlined in Supplementary Table 23 in their EHR on separate dates and possessing zero codes suggesting a possible history of bicuspid aortic valvular disease (Supplementary Table 24). Individuals were defined as not having TAAD if they had zero diagnosis or procedure codes suggesting a diagnosis of TAAD (Supplementary Table 25) and their EHR reflected two or more separate encounters in the VA Healthcare System in each of the 2 years before enrollment in the MVP. In the replication cohorts, TAAD definitions are described in Supplementary Table 22. The MVP received ethical study protocol approval by the VA Central Institutional Review Board, analysis in the UK Biobank was approved by a local institutional review board at Partners Healthcare (protocol 2013P001840), and informed consent was obtained for all participants. Additional information regarding experimental design and participants is provided in the Nature Portfolio Reporting Summary.
Stepwise conditional analysis
We used the COJO-GCTA software9 to perform an approximate, stepwise conditional analysis to identify independent variants within TAAD-associated loci. We used TAAD summary statistics from the overall meta-analysis to conduct this analysis combined with an LD matrix obtained from 10,000 unrelated, ancestry-matched (86% European, 10% African, 3.5% Hispanic) individuals from the Penn Medicine BioBank. Before this conditional analysis, we aligned our summary statistics with the ancestry-matched reference panel using the DENTIST software56. We set a threshold P < 5 × 10−8 (genome-wide significance) to declare statistical significance.
PheWAS of TAAD risk variants
The IEU OpenGWAS project13,14 is a publicly available online repository of a wide array of summary statistics from previously published GWAS and the UK Biobank. For TAAD lead variants identified in our GWAS analysis, we queried the phenotypes available in the IEU OpenGWAS project to perform a PheWAS12 across a range of over 2,000 conditions, diseases and metabolites. Details of the sensitivity analysis re-examining DBP and height-associated variants with TAAD accounting for blood pressure and height using individual-level data in the MVP are described in the Supplementary Methods.
TAAD risk factor Mendelian randomization analyses
MR analyses for smoking (through a lifetime smoking index), lipid levels (triglycerides, HDL and LDL cholesterol), blood pressure (SBP, DBP, PP and MAP) and height exposure were performed with TAAD as the outcome. Given that some of the above exposure summary statistics included UK Biobank data, the TAAD outcome summary data included all of the studies in our analysis except the UK Biobank, encompassing 12,422 TAAD cases and 578,768 controls. Genetic instruments were selected as DNA sequence variants that were associated with the exposure at genome-wide significance (P < 5 × 10−8) with an R2 < 0.001. All clumping was performed using the TwoSampleMR R package57. Genetic instruments were constructed for the lifetime smoking index (462,690 participants)17, lipid levels (up to 188,577 participants)18, blood pressure (up to 436,845 participants; https://pan.ukbb.broadinstitute.org) and height (253,288 individuals)19 using publicly available summary statistics (Supplementary Table 14). Inverse-variance-weighted MR was used for the primary analysis, with weighted-median20 MR performed as the sensitivity analysis, allowing for up to 50% of the weight of each instrument to be drawn from invalid instruments while controlling type I error. MR-Egger22 analysis was performed to evaluate for horizontal pleiotropy, as was the MR-PRESSO21 test, which consists of three parts: (1) the global test for horizontal pleiotropy, (2) the outlier-corrected causal estimate, which corrects for the detected horizontal pleiotropy and (3) the distortion test, which tests whether the causal estimate is significantly different after outlier adjustment. Given the high genetic correlation among blood pressure traits, we then used the MR-BMA methodology23 to generate multivariable models for analysis to prioritize the most likely causal blood pressure traits. Further details of the MR-BMA methods are contained in the Supplementary Information.
Causal TAAD gene and variant identification
We prioritized candidate causal genes at each of the identified TAAD risk loci by aggregating evidence from (1) prior genetic, clinical or functional studies, (2) the closest gene to the lead risk variant, (3) genes with protein-altering variants in high LD (R2 > 0.8) with the lead TAAD risk variant, (4) cis eQTL from the GTEx dataset in aortic tissue29 with association P < 5 × 10−6, (5) results from FOCUS28 version 0.5, a fine-mapping technique to identify causal genes in a TWAS58 using bulk RNA-seq data from post-mortem aortic tissue (387 individuals from GTEx) and TAAD meta-analysis (discovery and replication) summary statistics and (6) results of a colocalization analysis from our TAAD GWAS meta-analysis and eQTL data from GTEx bulk RNA-seq data in aortic tissue using the coloc R package59. Further methodologic details of these analyses and an analysis identifying putative causal TAAD risk variants are described in the Supplementary Information. Genes prioritized as causal (beyond FBN1 (ref. 24), ELN25, LRP1 (refs. 26,27) and TCF7L2 (ref. 5) where prior literature has established these as the likely causal genes) were identified based on having (1) three prioritization strategies highlighting it as a likely causal gene and (2) plausible biological evidence for a role in TAAD pathogenesis based on prior genetic, clinical or functional studie...
Comments
Post a Comment